Discussion
Thyroid cancer is the most common endocrine malignancy, though the mortality rate is relatively low (5-10%).
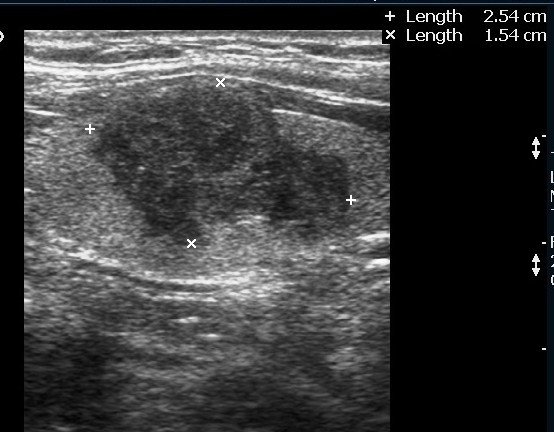
Ultrasound features suggestive of a malignant thyroid nodule include a solid, hypoechoic appearance, irregular margins, and absence of a hypoechoic halo. Hypoechoic lesions carry a higher risk of malignancy. Lymphadenopathy and local invasion of adjacent structures are highly specific for malignancy but are less frequently observed.
Follicular thyroid carcinoma (FTC), originating from follicular cells, is the second most common type of thyroid cancer, after papillary carcinoma, accounting for approximately 15% of all cases. FTC is a well-differentiated, slow-growing tumor that tends to spread hematogenously, commonly metastasizing to bone, liver, or lung. Regional lymph node metastasis is rare (incidence <10%).
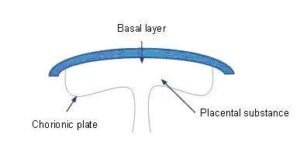
Follicular cell-derived thyroid neoplasms (adenomas and carcinomas) share overlapping clinical and cytological features, making it impossible to distinguish between them based on cytology alone. If fine-needle aspiration cytology (FNAC) suggests a follicular neoplasm, histopathology is required for a definitive diagnosis. The diagnostic criteria for follicular carcinoma are capsular and/or vascular invasion. Careful evaluation is necessary to differentiate foci of capsular invasion from capsular rupture due to FNAC penetration, which can result in worrisome histologic alterations following FNA of the thyroid (WHAFFT).
Follicular carcinomas are classified as:
- Minimally invasive follicular carcinoma
- Widely invasive follicular carcinoma
- Hurthle cell carcinoma (oncocytic)
- Insular carcinoma
Minimally invasive follicular carcinoma is well-encapsulated compared to the widely invasive variant. A diagnosis of minimally invasive carcinoma can be based on capsular invasion alone, vascular invasion alone, or both.
Hurthle cell variant
Hurthle cell carcinoma is often considered a variant of follicular carcinoma. Hurthle cell carcinomas are more likely than follicular carcinomas to be bilateral and multifocal, and they also have a greater propensity for lymph node metastasis.
Post-Operative Ultrasound
Postoperative ultrasound is used to:
- Evaluate the thyroid bed for residual disease.
- Detect local and nodal tumor recurrence.
Postoperative suture granulomas may appear as hypoechoic nodules with coarse echogenic foci and posterior acoustic shadowing in the thyroid bed. This appearance can mimic recurrent carcinoma.”
References
emedicine.medscape.com/article/278488
Prognosis of Patients with Papillary or Follicular Thyroid Cancer by Sheldon Rubenfeld, M.D.
http://www.endocrineweb.com/conditions/thyroid-cancer/thyroid-cancer-follicular
J Ultrasound Med. 2008 Oct;27(10):1431-7.PMID:18809953[PubMed – indexed for MEDLINE]
Tambouret R, Szyfelbein WM, Pitman MB. Ultrasound-guided fine-needle aspiration biopsy of the thyroid. Cancer. 1999;87:299-305. [PubMed]
Williams ED, Doinach I, Bjarnason O, Michie W. Thyroid cancer in an iodide rich area. Cancer. 1977;39:215-22. [PubMed]
Lin JD, Hsueh C, Chao TC, Weng HF, Huang BY. Thyroid follicular neoplasms diagnosed by high-resolution ultrasonography with fine needle aspiration cytology. Acta Cytol. 1997;41:687-91. [PubMed]
Yousem DM, Scheff AM. Thyroid and parathyroid. In: Som PM, Curtin HD, editors. Head and Neck Imaging. third edn. St Louis: Mosby; 1996. pp. 953-75.
Solbiati L, Livraghi T, Ballarati E, Ierace T, Crespi L. Thyroid gland. In: Solbiati L, Rizzatto G, editors. Ultrasound of Superficial Structures. London: Churchill Livingstone; 1995. pp. 49-85.
Simeone JF, Daniels GH, Mueller PR, et al. High resolution real time sonography of the thyroid. Radiology. 1982;145:431-5. [PubMed]
Solbiati L, Volterrani L, Rizzatto G, et al. The thyroid gland with low uptake lesions: evaluation with ultrasound. Radiology. 1985;155:187-91. [PubMed]
Propper RA, Skolnick ML, Weinstein BJ, Dekker A. The non-specificity of the thyroid halo sign. J Clin Ultrasound. 1989;8:129-32. [PubMed]
Noyek AM, Finkelstein DM, Kirsch JC. Diagnostic imaging of the thyroid gland. In: Falk SA, editor. Thyroid Disease: Endocrinology, Surgery, Nuclear Medicine, and Radiotherapy. New York: Raven Press; 1990. pp. 952-75.
Ahuja AT, Chow L, Chick W, et al. Metastatic cervical nodes in papillary carcinoma of the thyroid: ultrasound and histological correlation. Clin Radiol. 1995;50:229-31. [PubMed]